SOPORTE VITAL BASICO
(SEGÚN RECOMENDACIONES 2010 DEL EUROPEAN RESUSCITATION COUNCIL)
Medicina y Cirugía Oral y Maxilofacial: Medicina y Cirugía Oral y Maxilofacial
(SEGÚN RECOMENDACIONES 2010 DEL EUROPEAN RESUSCITATION COUNCIL)
Ver Artículo REGISTRO TERRITORIAL DE LA PROPIEDAD INTELECTUAL DE ARAGÓN Biblioteca de Aragón C/Doctor Cerrada 22, 3º Nº de Registro Salida: 284 Zaragoza 22 DE JUNIO DE 2017 FRANCISCO HERNÁNDEZ ALTEMIR FRAY LUIS AMIGÓ 8 -0 -B 50006.-ZARAGOZA
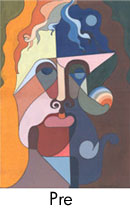
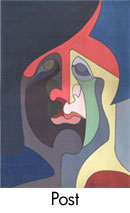
New device for submental endotracheal intubation
La cantidad de desviación septal observada después de la cirugía.
puede depender de la dirección y la magnitud de la
movimiento del maxilar durante la osteotomía LI. En consecuencia,
estudios previos revelaron que la dirección y el método
del movimiento maxilar con influencia de osteotomías LI
el área nasal y el tabique nasal. [23] Otra razón para
desviación septal después de osteotomías L1 es dislocación por un
brazalete parcialmente desinflado durante la extubación [24] e Ibrahim
et al.
[10] ofreció intubación orotraqueal submental
técnica (en la cual se coloca el tubo endotraqueal
directamente debajo de la barbilla) para evitar daños en el tabique nasal.
Además, esta técnica proporciona al cirujano
con una visión clara del campo quirúrgico, permite una fácil
visualización de cantos oclusales, líneas medias dentales, superior
altura del labio y no tiene efecto en ninguna estructura ósea. Eso
También permite la rinoplastia concurrente y ofrece una